In late August, on what was a muggy Miami summer
evening outside, among a whirl of activity, machine beeps and concerned faces, Dr.
Ciancio calmly led an entourage of his fellow surgeons still clad in surgery
scrubs following nearly 12 hours of surgery onto the 5th floor Pediatric
Intensive Care Unit; kindly introduced himself to his patient’s new nurse and
gave specific instructions for his care. His patient was Brennan. Hours earlier,
a living donor kidney was nestled in a stainless steel container and carried
from an immediately adjacent operating room and implanted by the highly capable
and talented hands of Dr. Ciancio into Brennan. That living donor was me, his
father.
There have been so many miracles along the way and this was a glorious culmination of so many people’s efforts and answered prayers. Medicine, we have learned, is a science and art at the same time sprinkled with educated guesses, calculated risks and cost/benefit ratios.
As a record breaking heat wave engulfed
much of the country this summer, we reached a critical crossroads in the care
of our son. His creatinine and blood urea nitrogen (BUN) had attained levels
approaching the need for dialysis and at this point the specter of hemodialysis
was lurking prominently in the background if a donor kidney was not located in
the very near future. All along, we intended for my kidney to be Plan B, but
after nearly 2 years on the transplant list with no calls for a suitable
cadaveric donor, we decided after consulting with Dr. P. to initiate the
process of giving him my kidney.
For the first three years of Brennan's life leading up to this
point, it felt like the beginning of a roller coaster ride while seated in the
front car, accentuated by a slow mechanical climb to a steep precipice with us
riding in the front car. When we made the decision that the time is NOW for
transplant, it was as if the first car of that roller coaster reached the
pinnacle of the track and it slowly creeped over the summit dangling there for
a brief moment to be followed by a sudden gravity wrenching descent with a
series of twists, turns and loops.
In that brief, lucid moment awaiting the rest of the cars to
clear the summit, we had a brief moment of a perfectly tranquil view of all of
the preparations we were going to make laid out below us, yet we were so high
the features below were not yet clearly defined. It was a moment of
unbelievable anticipation and hope. We had to make preparations medically by
making sure all x-rays, ultrasounds, blood work was current for both of us,
doctor approvals, family preparations during and after the surgery such as who
will help take care of who, how much school will Kyle miss, making sure our
employers support us... It was a long list of things to do and before we could take
another breath our brief moment of clarity was gone in a blinding rush and
things started happening alarmingly fast as the weight of the cars behind had
reached the point of no return as they cleared the top.
Nearly one year ago I had been approved as a donor for
Brennan but Dr. Ciancio wanted Brennan to be bigger for my kidney and now there were some tests that required repeating and subsequent
numerous visits to the hospital for both of us to confirm our status as being
compatible. Four days before surgery, I met with my surgeon, Dr. Chen and was
impressed at her knowledge and understanding of our situation. She explained
the procedure and how they were going to give Brennan my right kidney
necessitating an “open nephrectomy” translating into a larger incision, more
recovery time and the removal of part of my lowest rib. This rib does not connect to the sternum; instead it
juts out as a potential impediment to safely removing the kidney and could
tear the organ during removal. In the 60’s the removal of this rib served to enhance Hollywood starlets’
hour glass figures. The glue and internal sutures that would seal my incision
were designed to leave a minimal scar and can only withstand 10 lbs. per
square inch meaning I could not lift more than 10 lbs. for 8 weeks following
surgery. She told me I would be in a lot of pain; actually she told me I would
be in a hell of a lot of pain. Of course, my first thought was how much pain Brennan
will feel after surgery.
Her response hit me hard. She stated that he is sick. He has
been sick since he was born and he will begin to feel better immediately after
transplant. That simple statement, “he is sick”, weighed heavy on me and made
my eyes water. I was never in denial of his condition, but the possibility that
he will begin to feel better was the hope we have been clinging to these 3
years and it evoked my tearful response.
In the days leading up to the surgery, family began to
arrive to help as we made our final preparations. Going into this, I knew we
could not do this alone and that we were going to rely on our family and
prayers. I just never expected we would lean so heavily on them and just how
eager they were to help and how very capable they were of helping us pull
through.
One day prior to surgery, Brennan was admitted for IV fluids
to make sure he was sufficiently hydrated before surgery which was scheduled at
6 am the following morning. About 5:30 that morning the nurse entered our room
and informed us that the blood sample collected the evening before revealed his
platelet count is low-30! It should be a minimum 100 for surgery and this could
potentially delay surgery. A frenetic rush ensued to collect blood and analyze
the sample to determine if this was real or a lab error. After Brennan put up
his usual fight to resist the taking of the blood sample, the order “stat” was
placed on the vial and we waited. Soon, a young man still sleepy eyed, appeared
to transport Brennan to pre-op as the minutes passed we waited for the lab to
analyze this crucial sample. The nurse emerged and gave us the good news-
platelet count was over 200, the first sample must have been a lab error. The nurse handed the
transport guy his file and helped situate Brennan on the bed, Johely lay with him and we
were then hurried to the pre-op area.
In the pre-op area, a large room where the only privacy available came in the form of retractable curtains hung from the ceiling, I was peppered with numerous medical questions by a friendly nurse, an IV was started and told to change into a clean, standard issue blue hospital gown and hair net. When all standard preparatory procedures were finalized Brennan’s gurney was place next to mine, we tried to keep him occupied and our families were allowed in for pictures and prayers.
Next, a young surgeon emerged with a permanent blue marker
in hand to confirm the removal of my right kidney. He wrote “open” with his
initials on my right side, indicating the removal of my right kidney via the
open nephrectomy procedure. The surgical plan was to take Brennan first with a
staggered approach so that his kidneys could be removed and later sync with the
removal of mine. About 830 am he was taken into surgery. However, the actual
surgery does not begin immediately since there is still substantial preparatory
work to be completed while unconscious. A central IV line would be placed in
his neck for access purposes for fluids and blood samples; a breathing tube
place in his throat and a foley inserted to monitor urine production.
The removal of Brennan’s kidneys was necessary due to the
chance of infection from his urethral reflux. Removal means an extended
operation and recovery time. Typically, the ureter leads from the kidney and into the
bladder in a straight line. In Brennan, his looked like a spaghetti highway
acting as a potential harbinger for infection. Any possibility of infection (or
sickness) is not an ideal situation for transplant recipients due to the
immunosuppresants. Once ill, the patient usually goes to the hospital and an
intricate dance ensues balancing the reduction of immunosuppresants so the body
can fight the infection and not permitting the rejection of the transplanted
organ.
While Brennan was undergoing final preparations for surgery,
Dr. Ciancio emerged and informed us that his surgery would soon start and that
he was going to review my CT scan of my kidney again and that there was a
possibility they would take my left kidney instead. He explained my right kidney had 3 arterial
branches and if one of those clotted or became dehydrated in Brennan he could
potentially lose renal function in a part of the kidney, not to be reclaimed. Whereas, my left kidney had one arterial branch. He said he wanted this to be a 20 year kidney. With adult kidneys transplanted into pediatric patients,
proper hydration is essential and something we will diligently monitor.
Minutes later, Dr. Chen, appeared with a blue permanent marker in her hand. The decision to opt for my left kidney had been made, meaning a less painful and invasive laproscopic procedure. Unfortunately, my first foray into the realm of plastic surgery via the removal of my spare rib was not meant to be; no hour glass figure for me. I must admit having both sides of my abdomen marked in surgical permanent blue ink with no way to erase the instruction to remove my right and left kidney made me a wee bit nervous. I was assured by the attending, Dr. Chen that this would not be a problem since she was going to be doing the surgery. A futile attempt was made by a well-intentioned nurse to remove the marker but she only managed to smear it and she resorted to taping a piece of paper towel with the words “no” written on it.
After nearly four hours of Brennan in surgery and waiting
with my family in pre-op area my dance card was called at approximately 1230
pm. As I was being wheeled to the OR and laying on the gurney watching the
unremarkable hospital ceiling tiles pass by, the anesthesiologist must have administered
the sedative they promised and a nondescript friendly voice informed me Brennan
was in the adjoining OR. I said a quick prayer, to let him know that I love him
and was so proud of him and that I would see him soon. Nothing in the OR was
distinct at this point, just that someone was obviously moving my gurney into prime
cutting position, as far as I could tell, since I came in head first and now my
head was near the door. The ceiling
rotated and substantial surgical lights not yet turned on were poised in anticipation….
“Scott, wake up. You are out of surgery”, bellowed a demanding
male voice in an attempt to wake me as I was being pushed down the corridor
into post-surgical recovery. It was 6 pm. “Okay”, I groaned, with a shot of
pain crawling up my abdomen. Apparently, and no one informed me of this, once
out of surgery, you are woken up without pain medicine. Thus, the actual pain
from the surgery helps to wake the patient. Ouch.
In post-OR recovery, it was my not-so-good fortune to have
been assigned the world’s slowest pain medication nurse. As I writhed and
waited in pain from post-anesthesia side effect abdominal spasms (right where
it hurts!) and waited for this nurse to begin my morphine drip, the very
capable anesthesiologist came in to inform me that my kidney was successfully
placed in Brennan and producing urine!
Surgery for Brennan lasted another hour as his 6 inch scar
beginning below his sternum and extending just below his waist line was glued
and sutured internally. He was immediately admitted into the PICU while I was
relegated to the adult 6th floor post- surgery recovery.
The following day, partly due to some of
the medications Brennan was administered, he began to accumulate fluid in his
lungs. Attempts to dry out his lungs by placing an oxygen breathing tube under
his nostrils did not work because he was breathing with his mouth open. Further
measures, such as a fireman style oxygen mask were not successful from his open
reluctance to wearing such a mask. At this point, my Uncle Bill wheeled me over
to see him and Brennan looked good but not himself. His incision was larger than
mine and I ventured to guess he was in pain too. There was a total of eight IV
machines hooked to him forming a Christmas tree of blinking lights and numerous
tubes and lines in him. Looking at him for the first time post-transplant left
me speechless realizing that my kidney, a vital organ from me, was for him, a
remedy to finally feeling better. I think, in this brief moment, I understood
how a new mother must feel upon gazing at her newborn for the first time.
Assisting
my uncle in wheeling me to the PICU was my brother-in-law Bob. I marveled at
how, in the span of few short minutes he went from helping position my wheel
chair, to helping Johely with Brennan to offering comfort to Johely. In this
revealing moment he and my sister Amy, proved time and again to be our bedrocks
of support during our stay. Amazing familial support, to be sure.
During my visit, the fantastic head of PICU, Dr. Gelman
showed me X-rays of Brennan’s lungs and explained in great detail the
particulars of his condition and treatment. Going forward, the course of
treatment for the fluid in his lungs entailed the use of narcotic sedatives
with a breathing tube inserted in his throat and hand restraints to prevent him
from pulling out any tubes. These narcotics are highly addictive and led to a
longer stay in the PICU, since he would have to be weaned off gradually.
In the ensuing days, I was discharged after 3 days, and
there was a changing of the family guard as Bob and Amy returned home after
their nearly 9 day “vacation”, Johely’s mom came back down for a few days with Kyle (she had
gone back to our house with him to maintain some normalcy for his school and
schedule) and my cousin Leann helped attend Brennan’s bedside. All the while,
my Mom was present and helped me and Brennan to recover. Johely rarely left his side.
Each day for both of us marked improvement, some days better
than others. Brennan’s creatinine went from 4 prior to transplant, to 2.6
immediately after the surgery, 0.6 one week after transplant down to 0.3 after
about 10 days- Brenny’s kidney was working great! One of our favorite nurses
back at our regular hospital texted Johely and told her to call a number provided in the
text. When she called, it was evident she was on speaker and on the other line
were many familiar voices; she was speaking with all of Brennan’s regular
nurses at Miami Children’s Hospital. “Okay, tell us the creatinine.” Johely
responded with the low number of 0.3 and a cheer went up over the muffled
connection.
During a moment Johely and I will never forget, we
were sitting bedside with him and she was holding his hand (he really cherished everyone
holding his hand and we all took turns). He first turned to Johely and uttered,
“Thank you Momma.” Moments later he took my hand and repeated a similar
sentiment, “Thank you Da-da.” Wow. Was he really that aware at age 3 what he
had gone through and he had the presence of mind to thank us?
Soon, with his lungs clear, breathing tube removed and
coming off the narcotics we were to be transferred to the recovery floor for
transplant recipients as we started to see the familiar but “new” Brenny. On
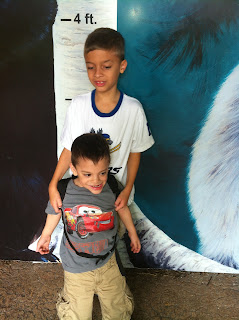
day 8 post transplant Brennan looked good enough to have a brotherly reunion with
Kyle and the familiar bond that ties them as brother was immediately evident
again as they both smiled and laughed for no other reason than being brothers
and boys.
The PICU, we have found, is the grinding stone of the
hospital; wearing you down with unrelenting stress, dimly lit rooms, constant
beeps and interuptions. Time here moves slowly and it is easy to lose track of the days with 2 days feeling like a week. Usually I am hesitant to name caregivers by name for
privacy issues, but these individuals are true professionals and deserve the
highest recognition in our opinion for their role in healing our son. This
stay, was made more tolerable by the many, many excellent and caring nurses and
doctors we met during our stay there; Dennis, June (with her kind smile), Sheila, Curt
(always looking out for Brennan’s best interests), Lynette and Sandra (amazing!). One particularly
warm story remains etched in our minds from his early days in the PICU. Sandra
a night nurse bathed, checked vital signs, monitored him through the night and
made Johely go to sleep. Johely swears Sandra didn’t take a break that evening;
all night constantly tending to Brennan.
After another 6 days on the recovery floor
and soon we were driving home for a reunion with Kyle. The adjustment at home
encompassed his new medications and his nutrition. Currently, he is on about 11
medications but this will reduce in the near future as he and the kidney grow
stronger but he will always be on immunosuppressants.
For the first month, following discharge we go three times
per week for blood work to make sure his immunosuppressants are at prescribed
levels. An adult kidney in pediatric patients needs to be sufficiently hydrated
which we can accomplish through his G-tube (tube in his stomach). However, he
needs to start eating by mouth and we will start speech therapy in the coming
days. Our challenges remain, but we will persevere with our faith, hope and
courage. Even now, we notice that Brennan is talking more and seems to have a
more favorable countenance.
On my first evening following my surgery, on
the 6th floor, a charge nurse entered my room and upon learning why
I was there scribbled on the board “Our hero.” I humbly submit that I am not
the only hero here and two quotes come to mind regarding this. The night prior
to surgery, I thanked my gathered family for their presence and help with
everything we were about to experience, to which Bob replied, “It takes a
village.”
A grandson of a World War II veteran once asked, “Grandpa, were you a hero in the war?” The once decorated brave soldier replied, “No…but I served in a company of heroes.” Obviously, organ donation is not akin to war but it is important to recognize all of the heroes who made this possible during our 18 day stay in the hospital and they all deserve praise and thanks!
Because Brennan received a living donor organ, in effect two
lives were saved on that day, August 21st. His life and the child’s life below him
on the transplant list, who maybe does not have the benefit of a close family
member genetic match now moves one step closer to a lifesaving transplant.
Those of you who have read this blog through the years
realize we have never used this as a political forum nor do we intend to do so
now. However, it is important to point out that in the recently passed Affordable
Care Act there are two key provisions that impact Brennan and could someday affect
your own son or daughter. First, there is a provision that prevents insurance
companies from imposing a “cap” on how much money a patient’s care may cost. If
there was a cap in place, I would not be writing this blog from a computer but
on cardboard on the side of the road begging for money.
Second, no denial for preexisting conditions by insurance
companies. Think about the hand we are dealt at birth and how much health can
be taken for granted. As a parent, I rest easier at night knowing my son will
not be prejudiced against by insurance companies for having a condition for
which he had no choice. Now if you are reading this you know someone who had an
organ transplant-please consider this when some politician tries to politicize
health care for the sake of another election cycle and ask yourself how would
you vote if you had a child or loved one with a chronic illness or special
need.
There is still work to be done as it concerns transplant
patient rights with glaring inequities in the system. This article is a perfect
description of that from the National Kidney Foundation website.
http://www.kidney.org/news/ekidney/august12/a_mothers_journey.cfm
In brief summation, it points out that Medicare does not
cover the cost of post transplant drugs 3 years after transplant and some
insurance companies choose not to cover these vital drugs. So instead of
spending $19,000 per year for the drugs, the patient goes back on dialysis
where the government picks up the tab at $77,000 per year. It is a short article
and well worth your time.
We considered changing the name of the blog
to “Brenny’s Bean” but the legal headache of going through all the paper work
was daunting. Not really, nothing trademarked here. Metaphorically, we like to
think of the Beans as all of you who have collectively helped us along the way.
Two of Brennan’s angels in particular, Dr. Ciancio and Dr. Paredes deserved the
highest praise and thanks. Without them and God, well we would not be here
right now. Thank you all and watch for the next exciting and hopefully shorter
blog entry coming soon! God Bless!!